In early 2022, the CDC published a report in the Morbidity and Mortality Weekly Report (MMWR) outlining findings from the HIV outbreak among people who inject drugs (PWID) in Kanawha County, West Virginia, from 2019–2021.
Read the full CDC report ➔ here
Key findings:
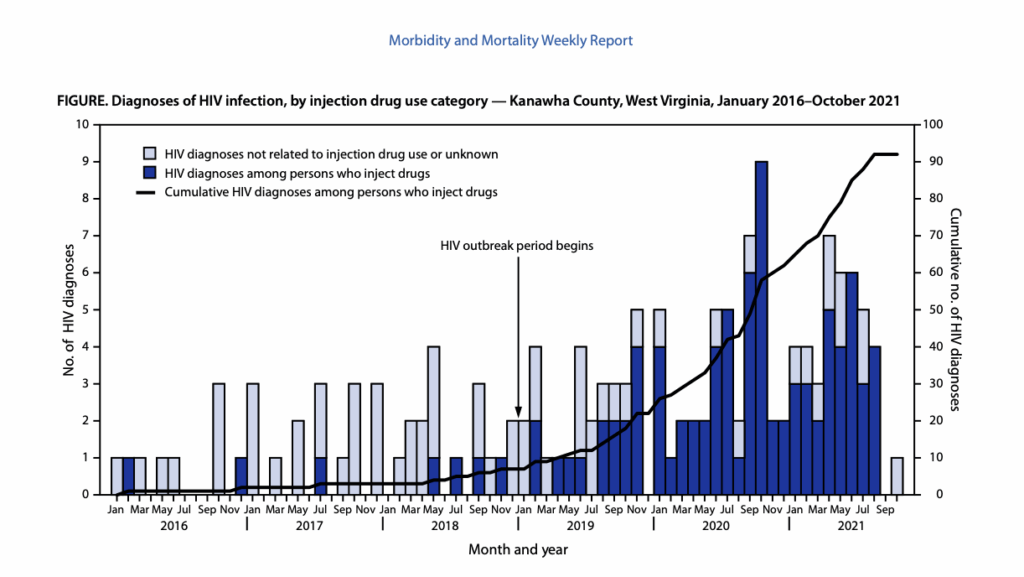
- Dramatic increase in HIV among PWID: After fewer than five cases per year during 2016–2018, diagnoses among PWID rose sharply to 85 cases by late 2021.
- Outbreak worsened after harm reduction closures: The suspension of syringe service programs (SSPs) in Charleston in 2018 and 2021, combined with stricter laws (like SB 334), left Kanawha without low-barrier syringe access during the outbreak.
- COVID-19 made the crisis worse: Pandemic restrictions cut back outreach, closed drop-in centers, and delayed HIV testing and care efforts.
- Severe impacts on the community:
- 47% of those diagnosed with HIV experienced unstable housing.
- 86% had a history of hepatitis C.
- Only 33% achieved viral suppression.
- Injection of methamphetamine and heroin was common, and syringe sharing rose after SSP closures.
- Deep stigma and mistrust: Many PWID avoided medical care after facing discrimination. Fewer than one-third were tested for HIV before their diagnosis despite frequent healthcare visits.
- Missed prevention opportunities: None of the patients had been prescribed PrEP (HIV prevention medication), and overdose prevention services like naloxone were underutilized.
CDC Recommendations:
- Expand low-barrier harm reduction services, including mobile and street outreach.
- Increase HIV and hepatitis C testing and treatment access.
- Reduce stigma among healthcare providers.
- Rebuild trust with PWID communities.
- Strengthen partner services (contact tracing and support).
Quote from the report:
“Stigma and discrimination and low SSP access have posed challenges to engaging PWID in HIV prevention and treatment; these challenges have been exacerbated by the COVID-19 pandemic.”
Learn more:


